A patient reported long-standing unilateral left nasal congestion and intermittent left-sided headaches. She had posterior rhinorrhea at times but not purulent drainage, itching or sneezing. Headaches were sometimes associated with intense nausea and vomiting.
Her allergy skin testing was positive to tree pollen, weeds and dust mite. 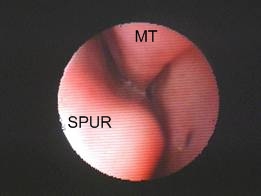 Nasal endoscopy shows a left septal spur abutting the middle turbinate(MT). Application of topical pontocaine led to significant reduction in headache. Sinus CT confirmed the findings and showed no other pathology. The patient’s pain resolved with septoplasty and partial turbinectomy.
Nasal endoscopy shows a left septal spur abutting the middle turbinate(MT). Application of topical pontocaine led to significant reduction in headache. Sinus CT confirmed the findings and showed no other pathology. The patient’s pain resolved with septoplasty and partial turbinectomy.
Facial pressure and nasal discomfort are common in patients with allergy and sinusitis but it is worth noting that a small subset of persons with those symptoms have rhinogenic migraine. This refers to a pain syndrome in which the principal cause is anatomic rather than infectious or allergic. It is believed that contact between two adjacent nasal structures is the source of the pain and if surgically corrected the pain will resolve.
Suspect rhinogenic headache in a patient whose pain seems out of proportion to the allergic/infectious findings. Examine the nose for a “contact point,” the presumed origin of the pain. Improvement with a topical anesthetic to the contact point might be helpful but it should not be considered a definitive diagnostic test. Obtain a sinus CT to better define the anatomy. Management is with a minimally invasive sinus technique (MIST).
Caveat: Even with a suggestive history as outlined above, a cure is not always possible with surgery. Headache syndromes are complex and sometimes multifactorial.
Reference:
Mariotti LJ, Setliff RC, Ghaderi M, Voth S. Patient history and CT findings in predicting surgical outcomes for patients with rhinogenic headache. Ear Nose Throat J. 2009 May;88(5):926-9.